The experience of menopause, the definitive biological transition marking the end of a woman’s reproductive years, is an absolutely universal and non-negotiable phase of the female lifespan. This profound change is far more complex than the cessation of menstruation alone, triggering a systemic, dramatic shift in hormonal balance that impacts nearly every major organ and physiological function.
Despite its universality and the profound medical consequences it entails, menopause has historically been sidelined in medical research and public health discourse. This neglect has created a significant, pervasive health gap in understanding, diagnosis, and effective treatment options for millions of aging women globally.
Addressing Menopause Health Gaps is the urgent, specialized discipline dedicated to advancing evidence-based care. It aims to improve clinical protocols, enhance patient education, and ensure that this critical life stage is met with proactive, comprehensive, and personalized medical management.
Understanding the vast, multi-systemic effects of estrogen decline, the specific health risks introduced, and the necessity of individualized therapeutic approaches is absolutely paramount. This knowledge is the key to minimizing suffering, safeguarding long-term health, and maximizing vitality during the second half of life.
The Biological Reality of Estrogen Withdrawal
Menopause is clinically defined as the point reached after a woman has experienced 12 consecutive months without a menstrual period. This transition is usually preceded by a period of several years known as perimenopause. Perimenopause is characterized by wildly fluctuating hormone levels and the onset of initial symptoms. The underlying biological event is the permanent decline in the production of estrogen and progesterone by the ovaries. This hormonal shift is the core driver of all menopausal symptoms and associated long-term health risks.
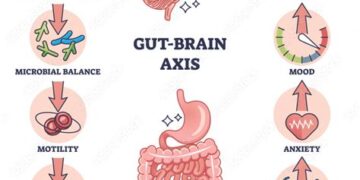
Estrogen is not solely a reproductive hormone. It is a powerful, protective chemical messenger with receptors present in the brain, heart, bones, and skin. Its withdrawal affects neurological function, metabolism, and cardiovascular health profoundly. The systemic nature of this hormonal change dictates that the medical consequences are wide-ranging.
The historical tendency to treat menopausal symptoms as merely temporary “hot flashes” represents a gross, dangerous oversimplification. This minimalization has obscured the serious, long-term health vulnerabilities introduced by estrogen deprivation. Effective care demands acknowledging the full, critical biological impact of this shift.
The health gap is perpetuated by a critical lack of dedicated medical training. Many primary care providers still lack the specialized education required to diagnose and treat complex menopausal symptoms effectively. This forces many women to navigate severe changes with inadequate professional support.
Cardiovascular and Metabolic Risk
The decline in estrogen levels is directly correlated with a significant and dangerous increase in a woman’s cardiovascular and metabolic risk profile. Estrogen loss removes a natural, powerful protective barrier against heart disease. This makes targeted intervention mandatory.
A. Cardiovascular Disease (CVD)
Estrogen withdrawal accelerates adverse changes in the lipid profile. It increases low-density lipoprotein (LDL, or “bad” cholesterol) and decreases high-density lipoprotein (HDL, or “good” cholesterol). This profile shift is a major risk factor for atherosclerosis and subsequent heart attack or stroke. Postmenopausal women experience cardiovascular events at rates comparable to men. This highlights the crucial nature of estrogen’s prior protective effect.
B. Hypertension and Vascular Function
The loss of estrogen negatively impacts vascular function. This leads to a measurable stiffening of the arteries and increased prevalence of hypertension (high blood pressure). Managing blood pressure rigorously through medication and lifestyle changes is paramount for mitigating future stroke risk. Active, continuous monitoring is essential for cardiovascular health.
C. Metabolic Syndrome and Weight Gain
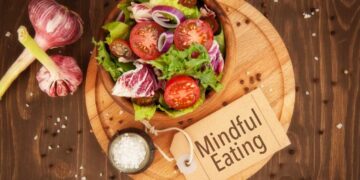
Menopause is frequently associated with unwelcome weight gain, particularly a dangerous shift in fat deposition toward the abdominal area. This visceral fat is metabolically active. It increases the risk of developing metabolic syndrome and insulin resistance. Dietary intervention and consistent strength training are critical for countering this adverse metabolic shift. Managing weight is essential for mitigating diabetic risk.
D. Increased Diabetes Risk
The cumulative metabolic changes—weight gain, increased visceral fat, and insulin resistance—collectively contribute to a substantial increase in Type 2 diabetes risk. Regular glucose screening and proactive dietary control are necessary preventative measures. Lifestyle modifications are the first line of defense against this severe metabolic consequence.
Musculoskeletal and Structural Integrity

The effect of estrogen withdrawal on bone density and muscle mass is another area of profound concern in menopause health. Estrogen is a key regulator of bone remodeling. Its absence leads directly to a heightened risk of structural breakdown and subsequent debilitating fractures. Maintaining structural integrity is crucial for functional independence.
E. Osteoporosis
The decline in estrogen significantly accelerates the rate of bone density loss. This loss leads directly to osteoporosis, a condition characterized by fragile, porous bones. Osteoporosis is a silent, progressive disease. It often remains undetected until a low-impact fracture occurs. The risk of hip and vertebral fractures is severe and life-altering.
F. Bone Density Screening
Bone Density Screening, typically performed via a DEXA scan, is a non-negotiable secondary preventative measure. Regular screening identifies bone loss early. It allows clinicians to intervene with specific medications (bisphosphonates) and supplemental calcium and Vitamin D to slow the rate of loss. Proactive measurement is essential for structural preservation.
G. Sarcopenia and Muscle Loss
Menopause often accelerates sarcopenia, the natural, age-related loss of muscle mass and strength. Maintaining robust muscle mass is essential for metabolic health, balance, and overall functional capacity. Resistance training becomes the most critical physical intervention. Consistent strength training is the best defense against mobility decline and falls.
H. Joint Pain and Inflammation
Many women experience generalized joint pain and stiffness during the menopausal transition. This discomfort is often linked to inflammation and changes in cartilage and connective tissue integrity driven by hormonal shifts. Management focuses on low-impact exercise, anti-inflammatory diets, and appropriate medication to maintain mobility. Maintaining flexibility is vital for quality of life.
Psychological and Cognitive Health
The hormonal fluctuations and eventual deficit profoundly impact psychological and cognitive health. These effects range from immediate, severe mood swings to long-term concerns regarding memory and sleep quality. These symptoms often cause severe disruption to daily life.
I. Mood and Affective Disorders
Severe mood swings, irritability, anxiety, and depression are common and debilitating symptoms during perimenopause and menopause. These affective disorders are directly linked to the rapid, unstable decline of estrogen and progesterone, which modulate key neurotransmitters. Proactive management involves therapy, stress reduction, and, in many cases, targeted medication or hormone therapy. The psychological burden can be severe.
J. Sleep Disturbances
Sleep disturbances, including severe insomnia and fragmented sleep, are a frequent complaint. These issues are often exacerbated by night sweats (vasomotor symptoms). Poor sleep quality severely degrades emotional regulation and cognitive function during the day. Addressing the underlying hormonal instability is crucial for restoring restorative sleep patterns. Sleep health is paramount for overall well-being.
K. Cognitive Function and Memory
Many women report temporary, troubling decline in cognitive function, often described as “brain fog” or short-term memory lapses. While these symptoms are generally temporary and not indicative of progressive dementia, they cause significant distress. Maintaining physical activity and rigorous mental stimulation helps support optimal brain health during this transition.
L. Vasomotor Symptoms (VMS)
Vasomotor Symptoms (VMS), or hot flashes and night sweats, are the most recognizable physical symptoms. VMS significantly disrupt sleep, concentration, and daily comfort. Treatment options range from lifestyle adjustments and specific non-hormonal medications to the highly effective use of Hormone Replacement Therapy (HRT). Management is essential for restoring basic daily comfort.
Conclusion
Menopause Health management is the critical, specialized field dedicated to mitigating the systemic effects of hormonal loss.
Estrogen withdrawal significantly accelerates critical cardiovascular risk, necessitating aggressive monitoring of blood pressure and cholesterol.
The decline in hormones mandates proactive intervention to mitigate severe, debilitating musculoskeletal risks like osteoporosis and bone fractures.
Rigorous Bone Density Screening (DEXA scans) is a non-negotiable secondary preventative measure required for identifying and treating early bone loss.
Consistent, structured resistance training is the most powerful physical strategy for combating muscle loss (sarcopenia) and maximizing functional independence.
Severe mood swings, anxiety, and profound sleep disturbances are significant psychological consequences that require specialized therapeutic support.
Vasomotor Symptoms (VMS) often necessitate targeted medical intervention to restore comfort and prevent fragmentation of necessary, restorative sleep.
The complexity of this transition demands that care be integrated, moving beyond simple symptom relief to address the entire multi-systemic impact of estrogen loss.
Understanding the biological necessity for targeted intervention is the only way to successfully overcome the historical neglect of this critical life stage.
Proactive, personalized management significantly reduces the incidence of chronic diseases and maximizes the period of functional independence.
Investment in specialized care is the ultimate key to bridging the knowledge gap and ensuring long-term health equity for aging female populations.
Tailored treatment ensures that women maintain vitality, optimal health, and structural integrity throughout the second half of life.